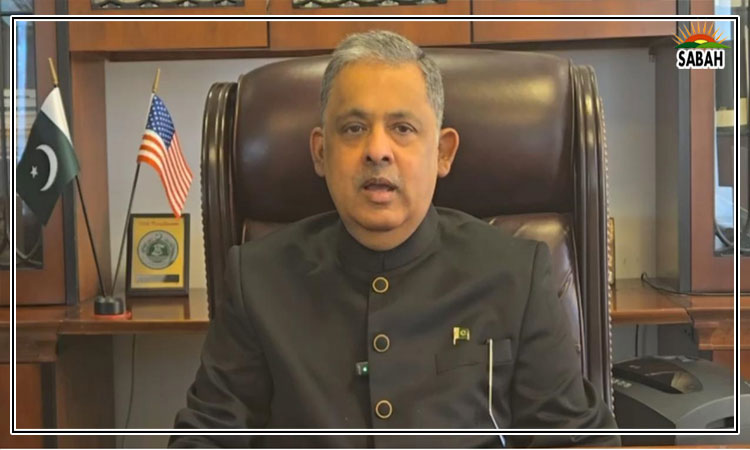
Physical health of mentally ill …..Zafar Mirza
Our bodies are gardens to the which our wills are gardeners. William Shakespeare
READERS might find it surprising to know that people with mental illness live less long than the general population. This is the case in every country. According to one study, people with severe mental illness live up to 25 years less than the general population. Why?
The high mortality rate among people with mental illness is not due to mental illness per se, rather it is the result of the coexistence or co-morbidity of physical health problems, such as cardiovascular, respiratory, metabolic and infectious diseases and cancer.
The Lancet, the oldest peer reviewed medical journal, set up a psychiatry commission which, in 2019, published a blueprint for protecting physical health in people with mental illness. Joseph Firth, Najma Siddiqi et al reviewed global evidence and reported that although for decades the higher prevalence of physical health issues among the mentally ill was well noted earlier it was thought that premature mortality occurs only among people with severe mental illnesses such as schizophrenia (a serious mental disorder) and bipolar disorders (people with severe mood swings of depression and euphoria) now there is evidence that individuals with any kind of mental disorder have a substantially reduced life expectancy. Indeed, suicide is more common among these people (disproportionately affecting young people and elderly women in low- and middle-income countries) as around 17 per cent of them die due to unnatural causes and it contributes to their relatively short lives.
The higher prevalence of physical health issues among the mentally ill have been well noted.
Research over the last two decades, though mostly in high-income countries, has shown that people with mental illness have up to double the chances of developing cardiometabolic diseases (a group of common but often preventable conditions including heart attack, stroke, diabetes, insulin resistance and non-alcoholic fatty liver disease) than those without mental illness. For patients with depression, the risk of developing cardiac disease, hypertension, stroke, diabetes, metabolic syndrome, or obesity is around 40pc higher than in the general population. Despite many research gaps, higher rates of infectious diseases like hepatitis B and C, HIV and syphilis are also found among people with mental illness. Research that followed those with severe mental illness over 10 years in Ethiopia noted individuals dying prematurely compared with the general population, and half of the deaths were from infectious diseases.
The reasons for the high prevalence of diseases and co-morbidity in people with mental illness and especially those among them with severe mental disorders are due to factors related to patients as well as to the healthcare system. People with mental illness have unhealthier lifestyles compared to the general population, for obvious reasons for example, self-neglect, smoking, sedentary behaviour and poor diet. These people are less able to access adequate healthcare than the general population. Even in a country like the US, people with severe mental illness are twice as likely as those without mental disorders to have been denied medical insurance because of pre-existing conditions. In low- and middle-income countries such as Pakistan, where access to healthcare generally and for the mentally ill in particular is inadequate, the situation is worse.
Some physical health problems in people with severe mental illness are associated with the use of medicines for the latter. The commonly observed physical side effects of these medicines include weight gain, menstrual disturbances, sexual dysfunction, muscle spasms, tremors, rigidity, restlessness, abnormal involuntary movements of different parts of the body for instance, the legs and lower jaw constipation, dryness of eyes, mouth and skin, blurred vision, slow heart rate, urinary retention, sedation and more. Management of these side effects poses a therapeutic challenge to these people.
The WHO estimates that more than 80pc of people with mental health conditions, including individuals experiencing neurological and substance use disorders, are without any form of quality, affordable mental healthcare.
A mentally ill person, especially one with schizophrenia, bipolar disorder or a major depressive illness, is most likely to carry a double burden of disease ie, mental illness and physical illness. But more often than not, physical illness accompaniments in mentally ill people are ignored. A mentally afflicted person is himself/herself unable to explain their physical illness under the effect of his/her mental illness.
The physical health of people with severe mental illness is also neglected in policies and research. People working on mental health are so challenged and occupied with the lack of mental healthcare for the mentally ill and there is so much to do in this regard that the physical health issues of mentally ill people remain under the radar.
Every column I write on almost any health issue in Pakistan, I come back again and again to the importance of primary healthcare as this is where the holistic and integrated delivery of quality health services must be reliably implemented. Now that, for the first time, mental health services have been included among the essential health services package for primary healthcare, it is time to provide proper training to health workers at primary care centres for taking care of mentally ill people including their physical health. Such trainings should also include how to identify signs of severe mental illness, and where required, how to counsel family members and where to refer such patients for advanced care of mental and physical illnesses.
It is heartening to note that attention is now being given to mental health training at the primary healthcare level. A major initiative has been taken to train general practitioners in this regard. More on this later.
As I mentioned earlier, most of the research on the physical problems of mentally ill patients, including those with severe mental illness, is done in high-income countries. Lately though, important work has been done in South Asia, including Pakistan, where for the first time these issues have been studied in the wake of Covid-19. More on this next time.
The writer is a former SAPM on health, professor of health systems at Shifa Tameer-i-Millat University and WHO adviser on UHC.
zedefar@gmail.com
Courtesy Dawn, March 24th, 2023