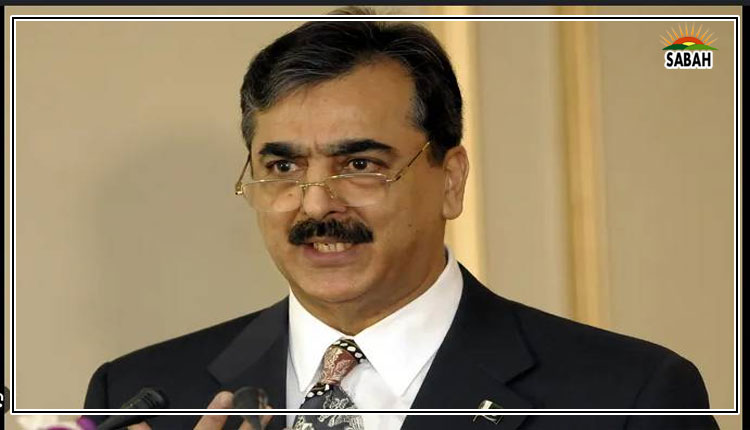
FAQs about universal health coverage…Zafar Mirza
DESPITE a simple-sounding concept, universal health coverage (UHC) is often misunderstood and misinterpreted at all levels, including among policymakers.
UHC is a national commitment under the Sustainable Development Agenda. Many countries, including Pakistan, have incorporated it in their national health policies and strategies. It is a simple concept without being simplistic, and is possible even in poor countries.
SDG-3 states: To ensure healthy lives and promote well-being for all at all ages. Target 3.8 under this goal reads: Achieve universal health coverage, including financial risk protection, access to quality essential healthcare services and access to safe, effective, quality and affordable essential medicines and vaccines for all. The deadline is 2030.
I have written on UHC in several of my articles in these pages, including The need for UHC literacy (Nov 19, 2021). There are, however, some frequently asked questions about UHC which I would like to clarify.
1. What is UHC? Under UHC, all people and communities can use the promotive, preventive, curative, rehabilitative and palliative health services they need, which are of effective quality. It also ensures that the use of these services does not expose the user to financial hardship.
UHC is a simple concept, without being simplistic, and is possible.
2. Can a country achieve UHC? There is no absolutism in UHC; it is a progressive universalism based on the right to health. It is never fully achieved but we can always advance towards it. Depending on their political choices, financial commitment and continuity, countries can progressively move towards UHC, provided there is a correct roadmap.
3. What is the correct roadmap for UHC in low- and middle-income countries (L&MICs)? UHC is a five-lane road. To start with, we need to be on the right road, which is equivalent to a clear policy vision. First, to select a minimum set of health services, which must be available to every citizen.
Second, strengthen qPHC (quality primary healthcare) because this is where the bulk of health service coverage can be provided. Third, prioritise those most in need and protect them from financial hardship in healthcare. Fourth, ensure the quality of healthcare.
Fifth, monitor and report progress for any course correction and ensure continued advancement and expansion. Poor countries need UHC more because of unattended healthcare needs and their negative implications for human capability and national economic development.
4. Whose responsibility is it to develop the UHC roadmap and how? It is the governments responsibility to construct this road and define the essential/minimum package of health services (EPHS), which is commensurate with the national burden of disease, and to finance its provision. The entire healthcare system must be aligned with the goal of reliable provision of this package to all people.
A robust and aligned health system to ensure EPHS provision includes good health governance, enhanced financing, a well-trained health workforce, reliable health information, availability of essential medicines, diagnostics etc, and digitisation of the healthcare system, with a focus on qPHC. Additional financing can be mobilised through fiscal prioritisation and innovative financing, instead of giving the excuse of lack of fiscal space. Looping in the private sector as a partner and continuously monitoring progress are essential conditions.
5. What minimum package and which health services? Backed by more than 25 years of health services research by World Bank and other agencies, there is now a better understanding about which are the essential and minimum services that a government must provide to its people to protect them from diseases and health risks, and effectively treat them through early diagnosis.
A nine-volume study was published in 2017 covering all major groups of diseases, including infectious, non-communicable, mother and child health, mental health, cancers, surgery etc. It is called Disease Control Priorities, third edition (DCP-3). Thousands of health services were reviewed for their relevance to the global burden of disease and cost-effectiveness and eventually a package of 218 essential health services was proposed for L&MICs that should be provided through government financing. Of these, 104 services are of highest priority, which is the minimum that all governments must provide. This is the model which L&MICs are urged to follow by developing their own national package of health services.
6. Are we talking only about curative health services? No, the DCP-3 package consist of preventive, promotive, curative, rehabilitative, and palliative health services. The integrated delivery of these services are at five levels of healthcare: community, first-level PHC facility, first-level hospital, tertiary-level hospital and population level (for instance, media campaigns on health education), can ensure an essential or minimum level of UHC.
Up to 90 per cent of these services can be provided at the first three levels and only 10pc of patients with advanced problems should be referred to tertiary-level hospitals. This is why qPHC and district-level healthcare are so important.
7. Has Pakistan developed these health services packages? Yes, it is the first country to follow DCP-3 guidance and has developed a National Essential Package of Health Services after robust efforts spanning three years. It was launched in October 2022 and contains 88 highest-priority health services which must be provided at the qPHC level and first-level hospitals. All provinces have also developed their own EPHS. These packages have been costed.
8. What about financial protection? Most L&MICs, like Pakistan, have mixed health systems and many patients go to the private health sector where they should be financially protected for the provision of EPHS by GPs through, for example, a government-financed health insurance system, like Pakistans Sehat Suhulat programme, which is currently limited to hospitalisation.
9. How to ensure quality in healthcare? By developing a national quality policy for healthcare, developing quality standards, training health professionals on compliance with these standards and by monitoring adherence.
10. Can UHC be monitored? Yes, through reliable collection of data on 14 proxy health services and health system indicators and calculating the UHC Service Coverage Index, which ranges from one to 100. Pakistans SCI in 2022 was 52.7. The 2030 target is to achieve an SCI of 80.
All resources mentioned in this article are available online.
Courtesy Dawn